The diagnosis of obesity is based on Body Mass Index (BMI).
BMI = Weight (kg)/ Height2 (m2)
- BMI = 19 – 25: normal body weight
- BMI = 25 – 30: overweight
- BMI = 30 – 40: obesity
- BMI = 40 – 50: morbid obesity
- BMI >50: super morbid obesity.
For example: A person with a height of 1.60 m is:
- Normal if the body weight is 49-64,
- Overweight if the body weight is 65-77,
- Obese if the body weight is 78-102,
- Morbid obese if the body weight is 103-127,
- Super morbid obese if the body weight is 128-153,
- Super super morbid obese if body weight is >154.
Is there any relation between Type 2 Diabetes and obesity?
Obesity causes accumulation of adipose tissue especially in and around intra-abdominal organs. The prevalence of obesity increased by 60% and of the diabetes mellitus by 90% in the last fifteen years in our country. Although the exact etiology of the diabetes is not known, it is acknowledged that obesity plays an important role in this increase. The most important evidence derives from the fact that the blood glucose is restored to physiological ranges, when the patients lose weight.
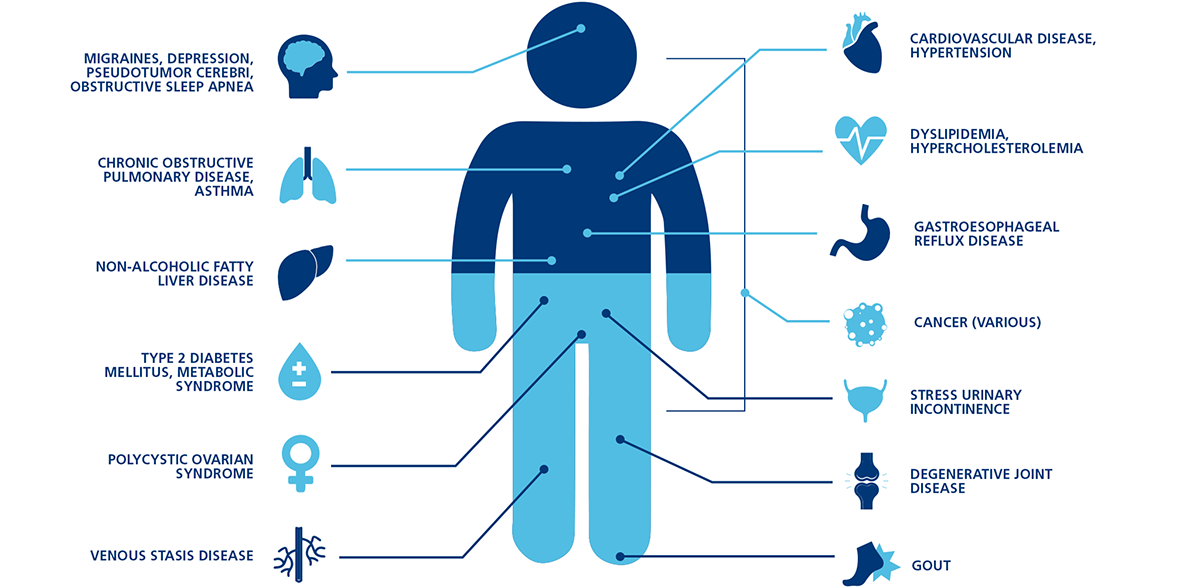
What are the risks related with obesity?
Obese patients live 10 to 15 years shorter relative to the mean life expectancy in the relevant country. Obesity is accompanied by various comorbidities such as:
- Type 2 Diabetes,
- Cardiovascular diseases,
- Hypertension,
- Stroke,
- Cancer (breast, prostate, esophagus, stomach, colon, uterus, kidney etc.),
- Pseudotumor cerebri,
- Sleep apnea, day time somnolence, chronic tiredness,
- Respiratory dysfunction,
- Depression
- Renal failure,
- Gout,
- Joint diseases (osteoarthritis, rheumatoid arthritis),
- Polycystic ovary syndrome,
- Congenital defects (neural tube defects),
- Infertility (applies to both genders)
- Delivery problems and gynecological complications,
- Urinary incontinence,
- Musculoskeletal system diseases,
- Carpal tunnel syndrome,
- Varicose veins,
- Deep vein thrombosis,
- Liver diseases,
- Gall bladder diseases,
- Pancreatitis,
- Impaired immune reaction,
- Wound infections,
- Gastro-esophageal reflux, hiatal hernia,
- Low back pain,
- Increase in surgical complications,
- Abdominal hernia,
- Skin diseases (fungus, acanthosis nigricans),
- Lymphatic circulation disorders (lymphedema, elephantiasis),
- Problems arising from abnormally enlarged breasts (mamomegalia): skin changes, breast pain, neck pain, chronic body odor, infections etc.
- Giant abdominal wall lumps (abdominal panniculitis, chronic infections, clothe problems, lumbalgia)
Who qualifies for surgery?
Each patient needs to be evaluated separately before surgery. A careful multidisciplinary evaluation, detailed examinations and tests should be carried out. The decision of bariatric and metabolic surgery is based on the international guidelines and ethical principles. A council composed of all departments participated in the treatment of the patient meets before operation and gives the final decision on approval of the surgery.
AGE:
Patients should be between 18 years to 65 years in order to be considered for surgery. However, there might be a need for surgery in the adolescence group as well. Nowadays, more and more adolescents are being operated. However, these patients are required to be carefully evaluated a pediatric endocrinologist in our team. Certain elderly patients over 65 may also be considered for surgery as well.
WEIGHT:
Body Mass Index plays the key role in selecting patients for obesity surgery:
- Patients with a Body Mass Index (BMI) >40 kg/m2, can be operated without a need for a comorbidity,
- Patients with BMI >35 kg/m2 should have at least one of the following conditions:
- Diabetes mellitus,
- Coronary artery disease,
- Polycystic ovary syndrome,
- Sleep apnea,
- Arthritis,
- High blood pressure,
- High cholesterol,
- Venous stasis disease,
- Soft tissue
Choice of the surgical method
Selection of the best surgical technique requires a detailed interview, physical examination, investigations and tests. The method is selected jointly with the patient and surgeon according to the needs. Here, the most common two methods are addressed. Selection of the method substantially varies for the patients with history of an obesity surgery.
Sleeve Gastrectomy
It is one of the most common methods. Closed or laparoscopic method is used for the sleeve gastrectomy, or in other words, the procedure is performed through holes as small as 5 to 12 mm in diameter. In the sleeve gastrectomy, the size of the stomach is reduced approximately by 75-80% using surgical staplers. Moreover, the entire staple line is manually sewn once more and a fibrin glue is sprayed over to boost the security. The resected stomach is removed without a need for an extra hole. The residual stomach measures approximately 100-150 ml in volume.
Gastric By-pass (Roux-en-Y Gastric Bypass)
Gastric bypass surgery is primarily preferred for patients with diabetes mellitus and metabolic syndrome. Gastric bypass is also the first option for patients with severe sweet eaters. As is the case with other methods, the procedure is carried out through small holes during the gastric bypass surgery. In a gastric bypass surgery, the volume of the stomach is reduced approximately to 25 to 30 ml. Next, a bypass route is created between the stomach and the small intestines. In the second phase, a second bypass tract is created between the small intestines.
Results of Bariatric and Metabolic Surgery
Sleeve gastrectomy results in a 70% excess weight loss, while 80% of the excess weight can be lost after a gastric bypass surgery. Many diseases improve in the postoperative period.
Resolution Rates after Bariatric and Metabolic Surgery:
- Type 2 diabetes (improvement or complete cure) 83%
- Decrease in risk of cardiovascular diseases 82%
- Hypertension 52-92%
- Sleep apnea 74-98%
- Pseudotumor cerebri 96%
- Hypercholesterolemia 63%
- Metabolic syndrome 80%
- Polycystic ovary syndrome 79%
- Varicose veins 95%
- Gout 77%
- Correction of urinary incontinence 44-88%
- Degenerative joint disease 41-76%
- Asthma 82%
- Depression 55%
- Reflux 72-98%
- Improved quality of life 95%
What to expect in treatment period?
Preoperative preparations for an obesity surgery are more comprehensive and detailed relative to many other surgeries. The measurement results, laboratory tests and examination findings are discussed in a council and the final decision is made on the method of treatment. The council consists of;
- Bariatric and Metabolic Diseases Surgeon,
- Endocrinologist,
- Nutrition Expert,
- Psychologist and Psychiatrist,
- Gastroenterologist,
- Pulmonologist,
- Cardiologist,
- Anesthesiology and Reanimation Physician,
- Gynecologist and Obstetrician,
- Coordination Nurse,
- Physicians of other relevant
Obesity surgery is safe
Metabolic Surgeries carried out to manage obesity and type 2 diabetes mellitus are quite safe procedures. Detailed preoperative examination, investigation and preparation boost the safety of such operations. The equipment available in the hospital, experience of the surgical team and proper postoperative monitoring minimize the risks. Most common complications of these procedures are listed below, although they are rare.
Complications:
- Bleeding
- Leaking on stapler line
- Deep vein thrombosis
- Pulmonary embolism
- Heart attack
- Intestinal obstruction
- Wound infection
- Incisional hernia
- Stenosis
Side Effects:
- Food sensitivity
- Tiredness
- Vitamin deficiencies
- Altered bowel habits
- Development of gallstone
- Hair